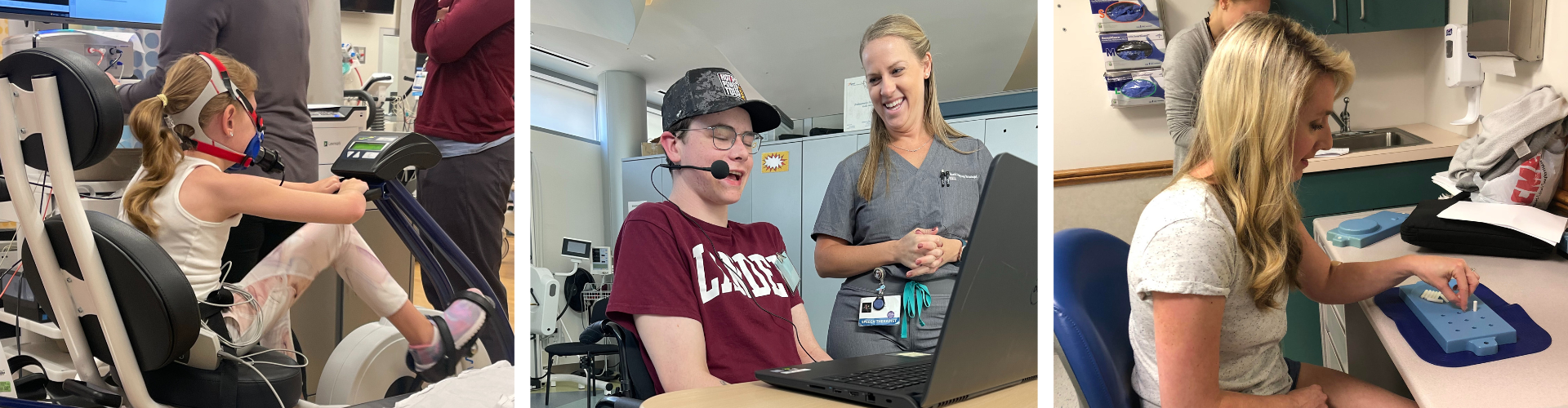
Your Role in Research
When you participate in a research study, you are volunteering to capture your experience with FA as data that can be analyzed. Clinical research can range from non-interventional studies that teach us more about FA in a person to interventional clinical trials that evaluate a new treatment approach.
Meet Shandra. In the video on the right, you can hear from a member of the FA community about the role she’s chosen to play in advancing FA research.